A universally accepted goal for most individuals is to have a long healthy lifespan. In order to do such, an optimally functioning cardiovascular system is a must, because this is the primary system that can provide the means to promote that long healthy lifespan. Cardiovascular disease is the primary cause of mortality in the elderly and accounts for the majority of deaths beyond age 65 years. However, the last statements might fool you into delaying necessary preventive adjustments until late in life, for the best means to treat the disorder should begin much sooner than waiting until the older age category is reached. One estimate is that elimination of cardiovascular disorders could increase life expectancy at least a decade. It is generally accepted by many that the key contribution to cardiovascular pathology in the elderly is systolic blood pressure (SBP) that characteristically increases as life progresses. Elevated SBP accelerates the physiological aging process in the circulatory system and is a major cause for strokes and progressive diminution of renal function. Interestingly, it has been abundantly mentioned in multiple reports that the harmful effects of the COVID-19 virus have been amplified time and again by elevated SBPs.
Recently, I was examining data on 725 non-diabetic volunteers for a number of clinical investigations. In this cross-sectional examination, 572 of them had recorded SBP readings. We use SBP here rather than diastolic (DBP) readings as most authorities believe the former is the greater provocateur of damage. From age 16 to 84 years, there was a gradual significant increase in SBP (p = <0.0001). In Fig. 1, data were divided into three age groups (16-40, 41-65, and 66-87 years). The linear lines of slope progressed in each group. Average SBP for 16-40 years was 114.8 + 1.02 (SEM), 121.6 + 0.89 (SEM) for 41-65 years, and 127.7 + 1.30 (SEM) for 66-87 years) a p values between each group of <0.0001 by ANOVA, Dunnett t test). [SEM=standard error of mean]
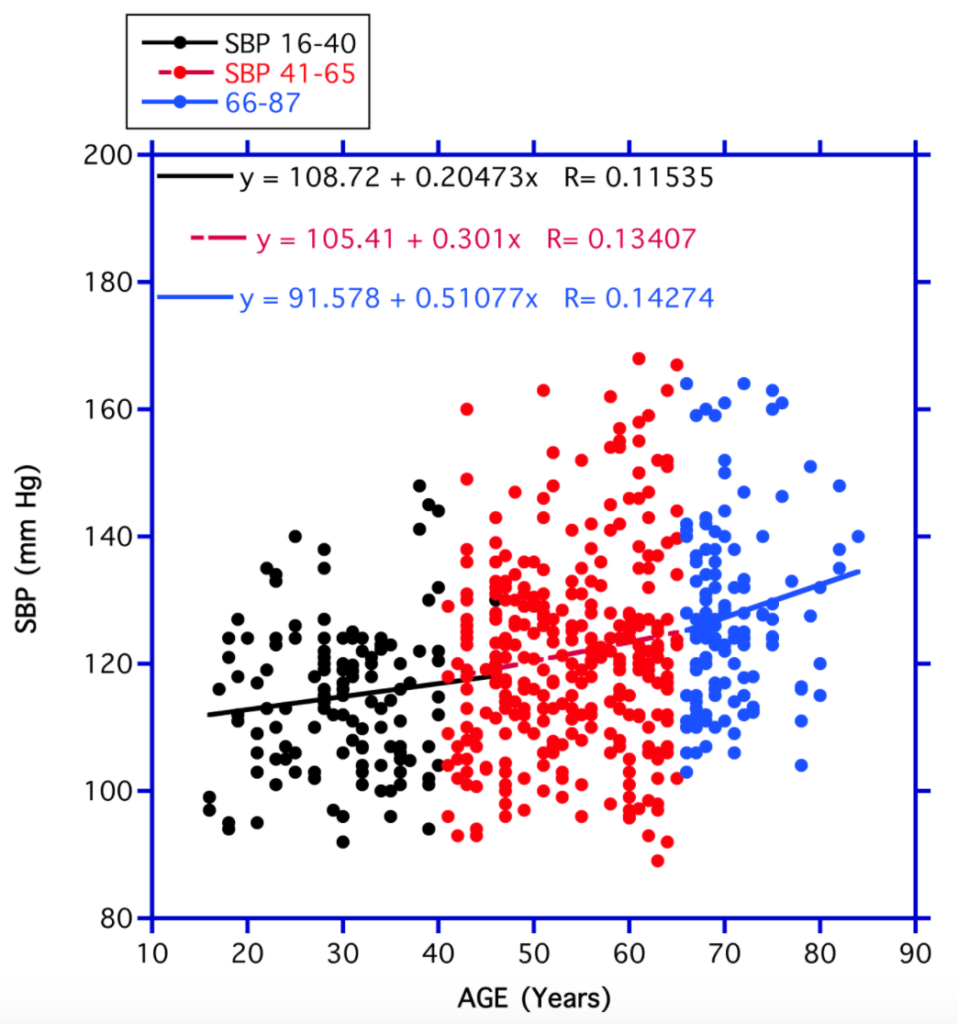
Remember, we are looking at so called “normal volunteers” required to be non-diabetic determined through examining a blood glucose level <125 mg/dl. Overall, the approximate average SBP rose from around average 116 mm Hg at age 16 years to average 138 mm Hg at 87 years. Is this average rise of 20 mm Hg a serious concern? One need only to examine well-funded studies involving thousands of individuals to determine that even small increments of SBP are harmful over the long run and suggest a necessity to find ways to improve these small differences (INTERSALT, INTERMAP). The final word — even minimal lowering of SBP, if consistent throughout a lifetime, can do wonders for overall health.
Are there any clues as to what we can do about this situation? Some so-called primitive societies (also referred to as non-modern, non-Western) in contrast to the modern industrialized world exhibit either virtually no change or perhaps even a slight drop in SBP with aging. Interestingly, higher SBP not infrequently develops if individuals from these primitive groups begin to develop a lifestyle similar to that of the more up-to-date world. Likewise, important to note, relocation of individuals from societies where low SBPs prevail to more present-day, modernized locations are frequently associated with progressive elevations of SBPs clearly indicating more factors than just genetic predispositions are involved. Can lifestyle be important in these matters?
The subject of BP elevations has become even more important due to links to the COVID-19 epidemic as mentioned above. Recent reports, even in younger victims, have mentioned a strong link between elevated blood pressures and the outcome of the infection. There seems little doubt that maintaining the most optimal SBPs over time can be helpful toward attaining a healthy long-term life span, especially during pandemics. While persistent improved lifestyle changes may be important, a need for easier, trustworthy approaches is warranted for most of the public – natural, safe supplements that bring on lower SBPs over the long term.
REFERENCES
Preuss HG, Aruoma OI: Suggestion for combatting COVID 19 by natural means in the absence of standard medical regimens. J Am Coll Nutr 2020 Jul @:1-3. Doi 10.1080/07315724.
Preuss HG, Mrvichin N, Kaats GR, Bagchi D: Reflecting on concepts relevant to contemplating the relationship between glucose/insulin perturbations and aging. J Am Coll Nutr. 38:463-469, 2019.
Preuss HG, Bagchi D: Chapter 10. Influence of dietary sugars on blood pressure regulation: historical, epidemiological, laboratory, and clinical considerations. In: Dietary Sugar, Salt and Fats, (eds) HG Preuss, D Bagchi, pp 219-250, 2020.
Intersalt Cooperative Research Group. INTERSALT: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Br Med J. 1988;297:319-328.
Dennis B, Stamler J, Buzzard M, et al. INTERMAP: the dietary data – process and quality control. J Human Hypertens. 2003;17:609-622.