In dealing with a variety of concepts to realize a safer, more healthful lifespan, I have long been intrigued over many years with the idea that a “Deadly Triangle” is a realistic hypothesis to examine in order to do such (Fig. 1). Because of this, I wrote my last report in the current series based on the deadly triangle. Simply put, among the many vital metabolic factors that exist, two appear especially important – insulin resistance and fat accumulation – regarding the latter, especially central fat accumulation (Fig. 1). Although I have used the deadly triangle at many symposia and written about it in a multitude of articles, I have always been intrigued with the top line of the figure and reported in the last article how both factors really simulated each other in their workings when compared. As suggested from the figure, I had assumed that the relationship between insulin resistance and visceral fat accumulation were bidirectional, even though there was no exact information to make such a supposition.
So, at that point, there was no definitive answer to the question whether insulin resistance drove body fat accumulation, body fat accumulation drove insulin resistance or as in the figure, there was reversibility between them. Why does it matter? It matters because the best way to prevent and/or treat any perturbation is to know as precise as possible its background pathophysiology.
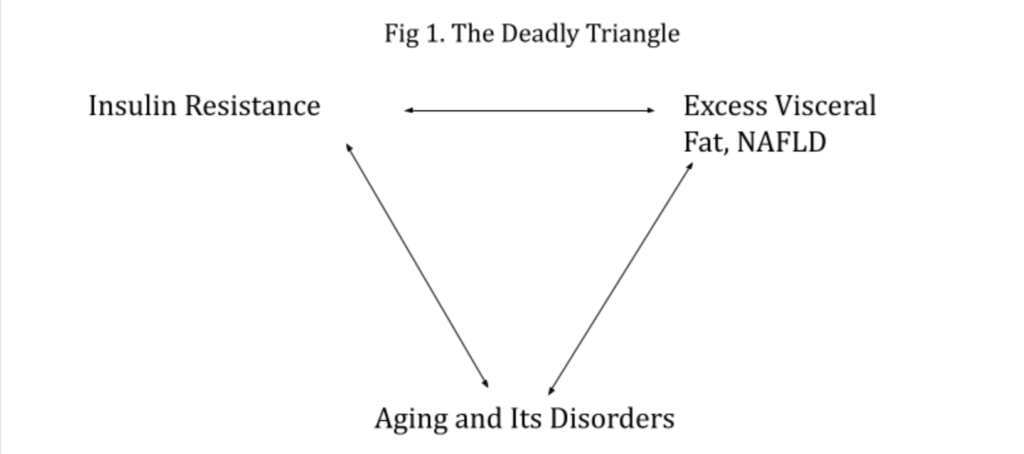
Going back to the last report, the new disclosure from that particular commentary was that visceral fat mass augmented inflammatory factors to a greater extent than insulin resistance. Nevertheless, whether one of the “two corner angles”, i.e., insulin resistance or central body fat mass, was more important than the other was not apparent in the majority of other respects. Since then, new information has come forth that further enlightens the relationship.
My current research examined how each of these two important factors influenced systolic blood pressure in non-diabetics where virtually all values fell into the normal range. Suffice it to say, essential hypertension is an important fact in the metabolic syndrome and aging. As expressed above, the question became how to determine, at least to some extent, the individual effects of each factor in the triangle.
Employing data from the last pool of volunteers, I recently began examining the correlation of circulating calcium levels with various metabolic parameters. Supplementation of calcium has been examined extensively regarding its ability to beneficially influence the extent of body fat mass as well as reduce blood pressure. Results in both positive and negative directions have been published [1-4]. The general consensus from these earlier reports is that calcium supplementation can result in body fat loss and blood pressure diminution, but the extent of this phenomenon is limited.
That’s where serendipity played its role. By chance when I examined the correlation of circulating calcium levels on both fasting blood glucose concentrations, a surrogate for insulin resistance, and body fat mass, I was quite surprised with the outcome illustrated in Fig. 2. Circulating calcium concentration obviously affected body fat mass significantly in a negative fashion, i.e., reduced body fat mass, but did not have a noteworthy influence on insulin resistance as represented by fasting blood glucose. As might be anticipated from our last report, hsCRP, a marker of inflammation followed fatty mass in revealing a decline with increasing calcium levels. Regarding our goal to determine the effects of each on systolic blood pressure, that measurement followed insulin resistance as there was no decrease in level.
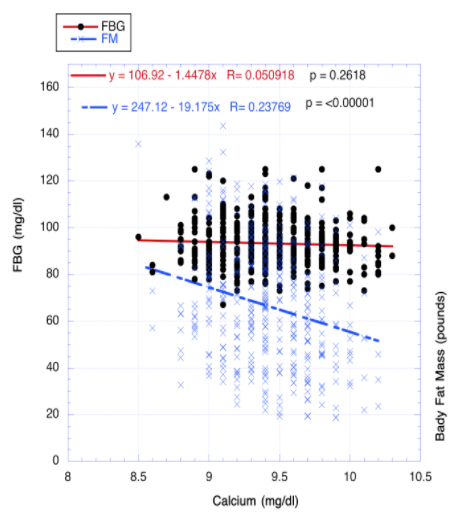
Accordingly, systolic blood pressure mainly follows insulin resistance, whereas inflammation is more directly affected by fat mass. Other aging parameters will be checked out using the above methodology. Therefore, treating both elevated insulin resistance and body fat mass appears to be the optimum choice for greater health as we delve further into the effects of each.